
Words have different meanings and can be confusing to a young child. It is likely that your child will hear standard medical expressions but not understand the meaning. Consider using child-friendly explanations when communicating with your child about their medical care. To ensure they are not misunderstood and that your child isn’t confused, here is some suggested language. Ideally, children should be asked if they know what the doctors or nurses mean when they say these words.
Medical expression: “The doctor will give you some ‘dye’.”
Your child may hear: “This is going to make me die?”
Suggested language: “The doctor will put medicine in the tube to be able to see your _____ more clearly.
Medical expression: “Shot”
Your child may hear: “Are they mad at me? When people get shot, they are badly hurt. Are they trying to hurt me?”
Suggested language: Instead of “shot,” refer to this as giving medicine through a small, tiny needle.
Medical expression: “CAT scan”
Your child may hear: “Will the be cats? Or something that scratches?”
Suggested language: Describe a CAT scan in simple terms such as “a machine that lets us see the inside of your body,” and explain what the acronym stands for.
Medical expression: “IV”
Your child may hear: “Ivy?”
Suggested language: Explain to your child that an IV is a tiny tube or straw that goes into their vein (hand) that gives their body water or it’s a fast way to give your child medicine.
Medical expression: “We’re going to take a picture.” X-rays, CT and MRI machines are for larger than a familiar camera, move differently and don’t yield a familiar end product.
Your child may feel like this: “I don’t feel like smiling.”
Suggested language: “These are machines that we use to take a picture of the inside of your body.” Describe the appearance, sound and movement of the equipment your child to help address any fears.
Medical expression: “We’re going to put you to sleep.”
Your child may hear: “Like my cat was put to sleep? It never came back.”
Suggested language: Explain that the medicine your child will be given will help them go into a very deep sleep. Explain that they won’t feel anything until the operation is over, and then the doctor will stop giving them the medicine so they can wake up.
Medical expression: “Take your vital signs.”
Child-friendly explanation: “We are going to measure your temperature and see how warm your body is.” Or, “We are going to see how fast and strong your heart is working.”
Medical expression: “Anesthesia”
Child-friendly explanation: Explain to your child that the doctor will give him or her medicine called ‘anesthesia’ and that it will help them sleep during their operation or procedure.
Medical expression: “Say goodbye to your parents.”
Child-friendly explanation: If you hear someone say this to your child, explain to your child that he or she doesn’t have to say goodbye but rather “see you later.” Explain to your child that you will see them in just a little while.
Hard or harsh term: “This will hurt.”
Child-friendly term: “You may feel very sore, achy, scratchy, tight, snug or full, etc.” Use manageable, descriptive terms. Words such as scratch, poke or sting might be familiar for some children and frightening to others.
Hard or harsh term: “The medicine will burn.”
Child-friendly term: “Some children say they feel a very warm feeling.”


 We will continue to discuss the different chapters from our digital
We will continue to discuss the different chapters from our digital 



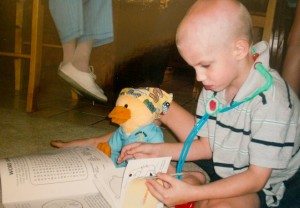

 During cancer treatment, a child’s appetite is so intermittent and unpredictable that it seems like food and eating become a minefield for parents to navigate. For the next few months, we are partnering with Melissa Sharp from Another Lunch to offer options and ideas to families living with this challenge. Her flair for nutrition and making food fun makes her the perfect fit for the series. Although the collaboration was conceived to assist children living with cancer, these ideas and recipes translate to any number of situations and illnesses that affect appetite. The topics for the series will include how to best add calories, encourage eating, reduce nausea, and ease sore mouths.
During cancer treatment, a child’s appetite is so intermittent and unpredictable that it seems like food and eating become a minefield for parents to navigate. For the next few months, we are partnering with Melissa Sharp from Another Lunch to offer options and ideas to families living with this challenge. Her flair for nutrition and making food fun makes her the perfect fit for the series. Although the collaboration was conceived to assist children living with cancer, these ideas and recipes translate to any number of situations and illnesses that affect appetite. The topics for the series will include how to best add calories, encourage eating, reduce nausea, and ease sore mouths.